Since its introduction in 2007, healthcare leaders have championed the Triple Aim, grappling with the challenges we know all too well today: curbing costs of care and advancing access to quality, safe, equitable, and evidence-based care. The revolutionary framework published in Health Affairs paved the path towards better health in this country but left out a vital component—the provider.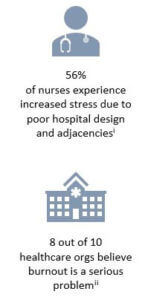
In this age of technologic evolution, reimbursement innovation, provider shortages, and epidemic rates of burnout, Bodenheimer and Sinsky saw the writing on the wall. We could not achieve the Triple Aim without recognizing that providers are patients, too, and that health systems cannot take care of populations without taking care of their own. The Quadruple Aim to improve the work life and wellbeing of the provider was thus introduced in 2014 in the Annals of Family Medicine.
The importance of the Quadruple Aim became more recognized as the ill-effects of provider burnout and fatigue on patient experience, quality, and safety became increasingly well-documented. While many of the interventions proposed are individually and internally focused (e.g. narrative medicine, journal clubs, yoga, meditation, and mindfulness), several pioneers have considered system-wide efforts, suggesting that hospitals and health systems would be remiss if they did not address the Quadruple Aim top-down, imagining an environment built for the 21st century provider in mind.
Healthcare is all about the patient populations we serve and the dedicated providers who care for them. As we plan for the future of healthcare, we believe it should be one where patients and providers come first—planning facilities that enable team collocation for improved workflow, collaboration and comradery, streamlined documentation, pre-visit planning, patient registration, and reduced barriers to practice top of license—providing space for respite and rejuvenation, and ensuring highest and best use of the built environment and the people that work there.
“Collegiality between colleagues is a necessary ingredient for team success. Teams that talk about their work are better able to accomplish goals. The experience of shared problem solving imbues teams with collegiality, making work easier and more enjoyable. And modern hospitals [have been] specifically designed to eliminate collegiality.” — Joshua Landy, MD, Founder of Figure 1
At Innova, we plan with the Quadruple Aim in mind. We work with clinical and administrative leadership alongside design teams to ensure the physical environment fosters health and well-being for both the healer and the sick; that the space planning make sense for the work life of modern-day clinician.
A few examples of caregiver support elements encompassed in our planning include:
- Evaluation and simulation of walking distances to reduce staff fatigue
- Access to natural light for providers
- Accounting for scribes in the ED and clinics to reduce documentation burden
- Incorporation of healthy food vending in staff break areas
- Inclusion of “caregiver support areas” that go beyond a typical break room
- Embedding “privacy enclaves” in team work-areas to enable private/quiet conversations within a collaborative zone
- Consideration of staff-convenience functions, such as daycare and exercise facilities, into master plans
How is your organization planning space to support your caregivers? Join the conversation below.
By Damiana Andonova | August 2019
[i] PriceWaterhouseCoopers. (2004). The role of hospital design in the recruitment, retention and performance of NHS NHS nurses in England. London: CABE. Retrieved from: https://webarchive.nationalarchives.gov.uk/20110118153647/http://www.cabe.org.uk/files/the-role-of-hospital-design.pdf
[ii] Swenson, S., Strongwater, S., & S, M. N. (2018). Leadership survey: immunization against burnout. NEJM Catalyst. Retrieved from: https://catalyst.nejm.org/survey-immunization-clinician-burnout/

